Condition
- Top tests
- Top tests
- Lifestyle Packages
- Lifestyle Packages
- Lifestyle Packages
- Top tests
- Diabetes
- Lifestyle Packages
- Diabetes
- Preventive Health Checkup
- Lifestyle Packages
- Lifestyle Packages
- Diabetes
- Diabetes
- Top tests
- Lifestyle Packages
- Top tests
- Top tests
- Lifestyle Packages
- Top tests
- Top tests
- Top tests
- Lifestyle Packages
- Infectious
- Preventive Health Checkup
- Diabetes
- Diabetes
- Preventive Health Checkup
- Top tests
- Top tests
- Heart Disease & Hypertension
- Lifestyle Packages
- Preventive Health Checkup
- Diabetes
- Diabetes
- Preventive Health Checkup
- Preventive Health Checkup
- Top tests
- Lifestyle Packages
- Diabetes
- Preventive Health Checkup
- Top tests
- Lifestyle Packages
- Diabetes
- Diabetes
- Diabetes
- Diabetes
- Diabetes
- Diabetes
- Preventive Health Checkup
- Preventive Health Checkup
- Diabetes
- Preventive Health Checkup
- Preventive Health Checkup
- Genomics
- Others
- Others
- Others
- Preventive Health Checkup
- Pulmonary / Infectious
- Diabetes
- Diabetes
- Others
- Preventive Health Checkup
- Others
- Preventive Health Checkup
- Top tests
- Others
- Genetics
- Others
- Gastrointestinal / Skeletomuscular
- Gastrointestinal / Skeletomuscular
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Others
- Top tests
- Top tests
- Top tests
- Top tests
- Top tests
- Top tests
- Top tests
- Top tests
- Top tests
- Preventive Health Checkup
- Top tests
- Top tests
- Top tests
- Top tests
- Blood Banking & Transfusion
- Lifestyle Packages
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Top tests
- Top tests
- Lifestyle Packages
- Diabetes
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Others
- Others
- Others
- Others
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Vitamin Deficiency
- Vitamin Deficiency
- Vitamin Deficiency
- Vitamin Deficiency
- Vitamin Deficiency
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Blood Banking & Transfusion
- Diabetes
- Diabetes
- Heart Disease & Hypertension
- Preventive Health Checkup
- Diabetes
- Preventive Health Checkup
- Preventive Health Checkup
- Diabetes
- Diabetes
- Heart Disease & Hypertension
- Top tests
- Heart Disease & Hypertension
- Diabetes
- Top tests
- Diabetes
- Heart Disease & Hypertension
- Lifestyle Packages
- Heart Disease & Hypertension
- Lifestyle Packages
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Lifestyle Packages
- Preventive Health Checkup
- Preventive Health Checkup
- Top tests
- Preventive Health Checkup
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Top tests
- Top tests
- Lifestyle Packages
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Top tests
- Heart Disease & Hypertension
- Preventive Health Checkup
- Diabetes
- Lifestyle Packages
- Heart Disease & Hypertension
- Top tests
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Diabetes
- Lifestyle Packages
- Preventive Health Checkup
- Diabetes
- Top tests
- Diabetes
- Allergy
- Heart Disease & Hypertension
- Diabetes
- Heart Disease & Hypertension
- Diabetes
- Lifestyle Packages
- Lifestyle Packages
- Top tests
- Preventive Health Checkup
- Lifestyle Packages
- Preventive Health Checkup
- Preventive Health Checkup
- Diabetes
- Top tests
- Heart Disease & Hypertension
- Preventive Health Checkup
- Top tests
- Heart Disease & Hypertension
- Lifestyle Packages
- Lifestyle Packages
- Diabetes
- Preventive Health Checkup
- Top tests
- Diabetes
- Top tests
- Preventive Health Checkup
- Preventive Health Checkup
- Preventive Health Checkup
- Diabetes
- Lifestyle Packages
- Lifestyle Packages
- Heart Disease & Hypertension
- Lifestyle Packages
- Heart Disease & Hypertension
- Lifestyle Packages
- Preventive Health Checkup
- Preventive Health Checkup
- Preventive Health Checkup
- Lifestyle Packages
- Top tests
- Lifestyle Packages
- Top tests
- Lifestyle Packages
- Top tests
- Diabetes
- Diabetes
- Others
- Blood Disorders
- Top tests
- Others
- Others
- Others
- Fever
- Fever
- Blood Disorders
- Blood Disorders
- Preventive Health Checkup
- Preventive Health Checkup
- Profile
- Kidney Disease
- Kidney Disease
- Diabetes
- Diabetes
- Heart Disease & Hypertension
- Preventive Health Checkup
- Lifestyle Packages
- Thyroid Disorder
- Diabetes
- Diabetes
- Diabetes
- Diabetes
- Diabetes
- Diabetes
- Diabetes
- Top tests
- Allergy
- Top tests
- Top tests
- Top tests
- Top tests
- Diabetes
- Top tests
- Diabetes
- Top tests
- Top tests
- Top tests
- Liver Disease
- Diabetes
- Top tests
- Vitamin Deficiency
- Top tests
- Top tests
- Liver Disease
- Top tests
- Top tests
- Top tests
- Anemia
- Anemia
- Anemia
- Diabetes
- Diabetes
- Anemia
- Top tests
- Top tests
- Top tests
- Preventive Health Checkup
- Thyroid Disorder
- Heart Disease & Hypertension
- Top tests
- Preventive Health Checkup
- Diabetes
- Heart Disease & Hypertension
- Top tests
- Fever
- Allergy
- Liver Disease
- Lifestyle Packages
- Heart Disease & Hypertension
- Top tests
- Arthritis
- Top tests
- Top tests
- Heart Disease & Hypertension
- Kidney Disease
- Preventive Health Checkup
- Allergy
- Top tests
- Lifestyle Packages
- Top tests
- Kidney Disease
- Top tests
- Lifestyle Packages
- Top tests
- Preventive Health Checkup
- Preventive Health Checkup
- Top tests
- Top tests
- Vitamin Deficiency
- Allergy
- Diabetes
- Top tests
- Top tests
- Top tests
- Top tests
- Heart Disease & Hypertension
- Allergy
- Top tests
- Preventive Health Checkup
- Top tests
- Top tests
- Infertility
- Top tests
- Lifestyle Packages
- Allergy
- Diabetes
- Heart Disease & Hypertension
- Lifestyle Packages
- Preventive Health Checkup
- Preventive Health Checkup
- Top tests
- Preventive Health Checkup
- Top tests
- Diabetes
- Top tests
- Infertility
- Top tests
- Thyroid Disorder
- Top tests
- Allergy
- Preventive Health Checkup
- Vitamin Deficiency
- Top tests
- Top tests
- Infertility
- Lifestyle Packages
- Diabetes
- Liver Disease
- Kidney Disease
- Vitamin Deficiency
- Top tests
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Top tests
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Heart Disease & Hypertension
- Infertility
- Heart Disease & Hypertension
- Vitamin Deficiency
- Vitamin Deficiency
- Arthritis
- Arthritis
- Top tests
- Top tests
- Lifestyle Packages
- Preventive Health Checkup
- Lifestyle Packages
- Preventive Health Checkup
- Vitamin Deficiency
- Top tests
- Lifestyle Packages
- Lifestyle Packages
- Preventive Health Checkup
- Top tests
- Preventive Health Checkup
- Top tests
- Heart Disease & Hypertension
- Infertility
- Top tests
- Top tests
- Preventive Health Checkup
- Lifestyle Packages
- Top tests
- PCOD
- Preventive Health Checkup
- Lifestyle Packages
- Preventive Health Checkup
- Top tests
- Fever
- PCOD
- Kidney Disease
- Top tests
- Top tests
- Preventive Health Checkup
- Preventive Health Checkup
- Liver Disease
- Thyroid Disorder
- Top tests
- Heart Disease & Hypertension
- PCOD
- Top tests
- Arthritis
- Preventive Health Checkup
- Kidney Disease
- Lifestyle Packages
- Top tests
- Allergy
- Top tests
- Top tests
- Diabetes
- Thyroid Disorder
- Preventive Health Checkup
- Top tests
- Lifestyle Packages
- Preventive Health Checkup
- Top tests
- Kidney Disease
- Liver Disease
- Infertility
- Top tests
- Anemia
- Top tests
- Top tests
- Top tests
- Preventive Health Checkup
- Bone Health
- Cancer
- Fatty Liver

Tests
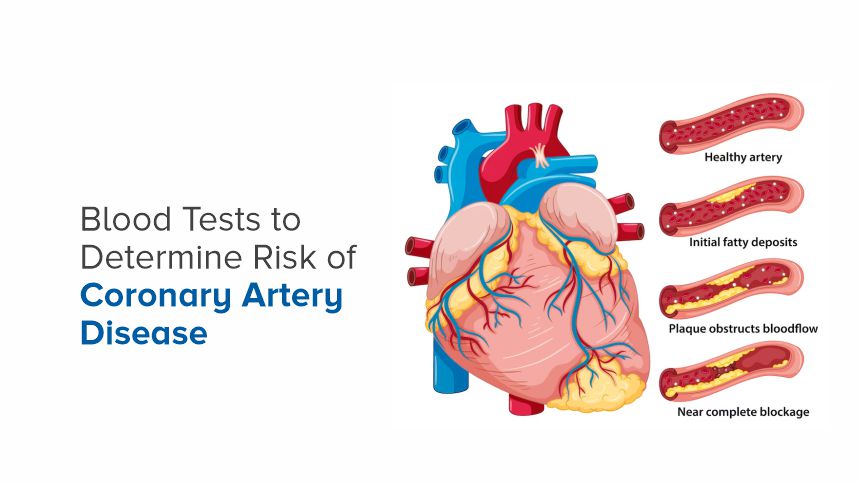
Ever wonder what secrets your blood might be hiding? It turns out, those red rivers coursing through your veins can reveal a great deal about your heart health. In fact, blood tests can be critical in determining your risk for coronary artery disease (CAD), a leading cause of death worldwide.
Here, we'll uncover how these tests work and why they matter to you. Whether you're a health enthusiast or just curious about keeping your ticker in top shape, understanding blood tests for CAD can provide peace of mind and vital knowledge for your well-being.
What is Coronary Artery Disease?
Coronary artery disease (CAD) occurs when the coronary arteries—the blood vessels that supply oxygen and nutrients to the heart—become narrowed or blocked due to plaque buildup. This limits the flow of blood to the heart muscle and can lead to chest pain (angina), heart attacks, and other serious complications. CAD is often referred to as a "silent killer" because it can develop over decades before noticeable symptoms appear.
The Importance of Early Detection
Early detection of CAD can significantly reduce the risk of severe complications. Blood tests are a non-invasive and effective method to catch early warning signs before the disease progresses. By identifying risk factors and biomarkers, these tests help doctors create personalized treatment plans to manage and mitigate the risk of CAD.
Cholesterol Levels and CAD
One of the primary blood tests for assessing CAD risk is the lipid panel, which measures cholesterol and triglyceride levels in your blood. High levels of low-density lipoprotein (LDL) cholesterol and low levels of high-density lipoprotein (HDL) cholesterol are associated with an increased risk of CAD. Regular monitoring of your cholesterol levels can help you and your healthcare provider take proactive steps to maintain a heart-healthy lifestyle.
LDL Cholesterol: The Bad Guy
LDL cholesterol is often dubbed the "bad" cholesterol because it contributes to plaque buildup in the arteries. When LDL levels are high, it can lead to atherosclerosis, making it harder for blood to flow through the arteries. Lowering LDL cholesterol is a key goal in reducing CAD risk.
HDL Cholesterol: The Good Guy
HDL cholesterol, on the other hand, is known as the "good" cholesterol. It helps remove LDL cholesterol from the bloodstream, transporting it to the liver for processing and excretion. Higher levels of HDL cholesterol are associated with a lower risk of CAD.
Triglycerides and Their Role
Triglycerides are a type of fat found in the blood. Elevated triglyceride levels can also contribute to plaque buildup and increase the risk of CAD. A lipid panel measures both cholesterol and triglyceride levels to provide a comprehensive picture of your cardiovascular health.
Inflammatory Markers and CAD
Inflammation plays a significant role in the development of CAD. Blood tests that measure inflammatory markers can help assess your risk. These markers include C-reactive protein (CRP), fibrinogen, and interleukin-6 (IL-6).
C-reactive Protein (CRP)
CRP is a protein produced by the liver in response to inflammation. Elevated CRP levels are associated with an increased risk of CAD and other cardiovascular diseases. High-sensitivity CRP (hs-CRP) tests are commonly used to evaluate CAD risk, as they can detect lower levels of CRP in the blood.
Fibrinogen and Blood Clotting
Fibrinogen is a protein involved in blood clotting. Elevated fibrinogen levels can indicate an increased risk of blood clots, which can lead to heart attacks and strokes. Monitoring fibrinogen levels can help assess CAD risk and guide treatment strategies.
Interleukin-6 (IL-6)
IL-6 is a cytokine that plays a role in the body's inflammatory response. Elevated IL-6 levels are associated with an increased risk of CAD. Testing for IL-6 can provide additional insights into your inflammatory status and cardiovascular health.
Blood Sugar Levels and CAD
Diabetes and elevated blood sugar levels are major risk factors for CAD. Blood tests that measure glucose and hemoglobin A1c (HbA1c) levels are essential for assessing diabetes and prediabetes, which can increase the risk of CAD.
Fasting Glucose Test
A fasting glucose test measures your blood sugar levels after an overnight fast. Elevated fasting glucose levels can indicate diabetes or prediabetes, both of which are associated with an increased risk of CAD.
Hemoglobin A1c (HbA1c)
The HbA1c test provides an average of your blood sugar levels over the past two to three months. Elevated HbA1c levels indicate poor blood sugar control and an increased risk of diabetes-related complications, including CAD.
Insulin Resistance and CAD
Insulin resistance, a condition in which the body's cells do not respond effectively to insulin, is a precursor to type 2 diabetes and is associated with an increased risk of CAD. Blood tests that measure insulin levels and insulin resistance can help identify individuals at risk and guide preventive measures.
Kidney Function and CAD
Kidney function is closely linked to heart health. Blood tests that assess kidney function, such as creatinine and estimated glomerular filtration rate (eGFR), can help evaluate your risk of CAD.
Creatinine Levels
Creatinine is a waste product produced by the muscles and filtered out of the blood by the kidneys. Elevated creatinine levels can indicate impaired kidney function, which is associated with an increased risk of CAD.
Estimated Glomerular Filtration Rate (eGFR)
The eGFR test estimates how well your kidneys are filtering blood. A lower eGFR indicates reduced kidney function and an increased risk of cardiovascular complications, including CAD.
Albumin-to-Creatinine Ratio (ACR)
The ACR test measures the amount of albumin (a protein) in your urine. Elevated ACR levels can indicate kidney damage, which is associated with an increased risk of CAD. Monitoring ACR levels can help identify individuals at risk and guide treatment strategies.
Genetic Markers and CAD
Genetic factors can play a significant role in your risk of developing CAD. Blood tests that analyze genetic markers can provide insights into your inherited risk and guide personalized prevention and treatment strategies.
Familial Hypercholesterolemia (FH)
FH is an inherited condition characterized by extremely high levels of LDL cholesterol. Genetic testing can identify individuals with FH, allowing for early intervention and aggressive treatment to reduce the risk of CAD.
Apolipoprotein B (ApoB)
ApoB is a protein involved in the metabolism of lipids and is a component of LDL cholesterol. Elevated ApoB levels are associated with an increased risk of CAD. Genetic testing can identify variations in the ApoB gene that may contribute to CAD risk.
Lipoprotein(a) [Lp(a)]
Lp(a) is a type of lipoprotein that can contribute to plaque buildup in the arteries. Elevated Lp(a) levels are associated with an increased risk of CAD. Genetic testing can identify individuals with elevated Lp(a) levels, allowing for targeted prevention and treatment strategies.
Nutrition and Lifestyle Factors
While blood tests provide valuable insights into your risk of CAD, nutrition and lifestyle factors play a crucial role in managing and reducing that risk. Adopting a heart-healthy diet, engaging in regular physical activity, and avoiding smoking can significantly improve your cardiovascular health.
Heart-Healthy Diet
A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help reduce your risk of CAD. Limiting saturated fats, trans fats, and added sugars can also support heart health.
Physical Activity
Regular physical activity, such as brisk walking, running, or cycling, can help lower your risk of CAD. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity each week.
Smoking Cessation
Smoking is a major risk factor for CAD. Quitting smoking can significantly reduce your risk of heart disease and improve your overall health. Seek support from healthcare professionals, smoking cessation programs, or support groups to help you quit.
Monitoring and Managing Blood Pressure
High blood pressure (hypertension) is a significant risk factor for CAD. Regular monitoring and management of blood pressure can help reduce your risk of heart disease and related complications.
Blood Pressure Measurements
Blood pressure is measured using a sphygmomanometer, which provides readings of systolic and diastolic blood pressure. Normal blood pressure is typically around 120/80 mmHg. Elevated blood pressure readings may require lifestyle changes or medication to manage.
Lifestyle Changes to Lower Blood Pressure
Lifestyle changes such as reducing salt intake, maintaining a healthy weight, and engaging in regular physical activity can help lower blood pressure and reduce your risk of CAD.
Medications for Hypertension
If lifestyle changes are not enough to control blood pressure, your healthcare provider may prescribe medications such as diuretics, ACE inhibitors, or beta-blockers to help manage hypertension and reduce CAD risk.
Conclusion
Blood tests offer a window into your heart health, revealing critical information about your risk of coronary artery disease. From cholesterol levels and inflammatory markers to genetic factors and kidney function, these tests provide valuable insights that can guide personalized prevention and treatment strategies.
By understanding your risk factors and taking proactive steps to manage them, you can significantly reduce your risk of CAD and improve your overall cardiovascular health. Don't wait until symptoms appear—take control of your heart health today. Consult with your healthcare provider to discuss which blood tests are right for you and how you can incorporate heart-healthy habits into your daily routine.
WANT TO BOOK HEALTH CHECKUP ?
Categories
Top tests
114
Lifestyle Packages
47
Diabetes
58
Preventive Health Checkup
60
Infectious
1
Heart Disease & Hypertension
38
Genomics
1
Others
81
Pulmonary / Infectious
1
Genetics
1
Gastrointestinal / Skeletomuscular
2
Blood Banking & Transfusion
16
Vitamin Deficiency
12
Allergy
9
Blood Disorders
3
Fever
4
Profile
1
Kidney Disease
8
Thyroid Disorder
5
Liver Disease
6
Anemia
5
Arthritis
4
Infertility
6
PCOD
3
Bone Health
1
Cancer
1
Fatty Liver
1